


The Clinical Director for Jersey's new hospital project has defended the lower number of beds it will provide, saying changes in healthcare have reduced the length of time patients need to stay in hospital, and in some cases, avoided it altogether.
Professor Ashok Handa was addressing concerns after a letter from the Deputy Chief Minister, Senator Lyndon Farnham, to Scrutiny revealed that some services would have fewer beds available than they do in the current hospital.
He explained that a lot of things have changed in healthcare since the previous hospital was built, which “Jersey hasn’t really kept pace with”.
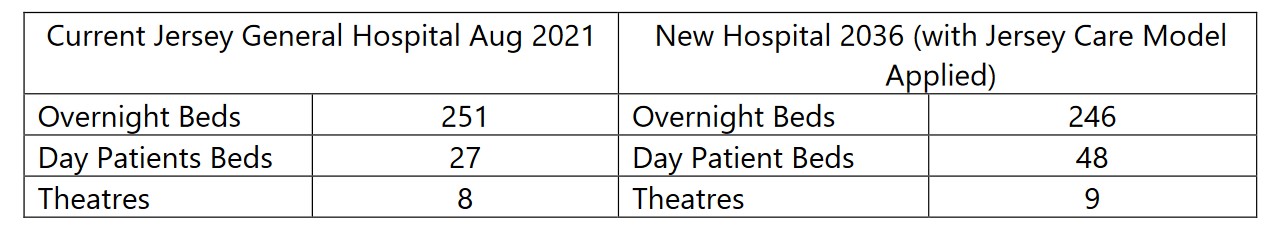
Pictured: A comparison of the number of beds available in the current hospital and proposed in the new one.
“Although people are comparing the current hospital and the hospital project, what they are calling bed is a is a fluid concept in healthcare,” he said.
“If you are talking about inpatient beds, the new hospital will have a whole variety of beds, day-case beds, treatment beds for oncology, for renal, for acute care, children's beds, obstetrics and maternity beds and critical care beds.
“And then, we have ambulatory care, where we have what we call an acute assessment unit, where people come in, and instead of waiting two or three days in the hospital to have tests, or a physio, you make sure all of those are in one place and you could have the test straight away, decisions made on treatment, the physio, OT, the meds and antibiotics all of that prepped up, and you can still go home 12 hours later, where currently, that same patient might be in hospital for three or four days.”
In addition, a number of surgery which used to require a patient to stay in hospital for the day or more, are now in ambulatory care in the minor operations outpatient service.
“An example of that is vascular surgery where people have an operation and the modern way of thinking is with endovenous laser treatment or radio frequency ablation, or injections, which is done as a clinic-based procedure,” Professor Handa said.
“Things like cystoscopy, people will come in and they're often given an anaesthetic to have a look of the telescope into the bladder, anow with flexible cystoscope you can those done, again, under local anaesthetic in the clinic setting.
“The way we're delivering health care for the hospital is very different and so we have all of these other facilities which currently would be done out of the bed base done in other parts of the hospital. The main message there is the hospital is much more than just the number of beds. It's a diagnostic, treatment and health center, all of that treatment, diagnostic, outpatient, ambulatory as well as some inpatient care.”

Pictured: Less procedures now require a patient to stay in hospital.
The same rational applies to beds available in the mental unit, which will be 10 less than currently available. Professor Handa explained that with a bigger focus on prevention, which involves investment in the talking therapies and outpatient consultations, fewer beds will be required.
In addition, thanks to “big enhancements in the community mental health nurses”, people will be able to get out as soon as they are safe to be home and have the right support.
While most of the wards will have less beds than currently, the private patient unit will have more, in a bid to ensure islanders who have private insurance use the local facilities, instead of going to the UK or not using their private insurance because they don’t see the benefits.
“It's not an increase, it's providing a much needed and better facility for the patient,” Professor Handa said.
“It’s not going to be a burden on the public purse, because more money will descend on public health because those who have insurance or personal means will use it, because the facility was good enough on island to use it, and those currently go off island will be able to stay on island for more treatment.
“That's the business model and the rationale behind building that, keeping the patients on Jersey, the Jersey pound on Jersey, and it's all also bout providing a facility so that people can use the insurance they pay for already.”
Professor Handa is currently working with clinicians to finalise the design brief of the project. He said he has been challenging the needs expressed by the teams to ensure the project does not waste money.
The final design brief will be shared as part of the planning application for the future hospital in November.
“My job is to run that tightrope between making sure that the hospital is big enough and is future-proof for the needs of the island; and at the same time, making sure, it's not too big and the facilities aren’t too luxurious, so that they're affordable by the public purse.
“That period, that process of challenge carries on all the way through the design process. As we get down to the next stage of design, from the biggest picture to the smaller picture to the department, down to the root down to what's going to be inside the room.”
Comments
Comments on this story express the views of the commentator only, not Bailiwick Publishing. We are unable to guarantee the accuracy of any of those comments.