

A “minority” of batches of donor blood used to treat Jersey patients over a 30-year period were “infected”, leading some to contract blood-borne diseases, the Health Minister has confirmed.
The revelation came amid questioning of Deputy Richard Renouf by Deputy Inna Gardiner, who asked about whether Jersey was affected in the blood contamination scandal spanning the 1960s to early 1990s, which is currently being investigated in a UK inquiry.
The scandal saw thousands of patients with haemophilia and other bleeding disorders infected with Hepatitis B and C, as well as a number of other viruses.
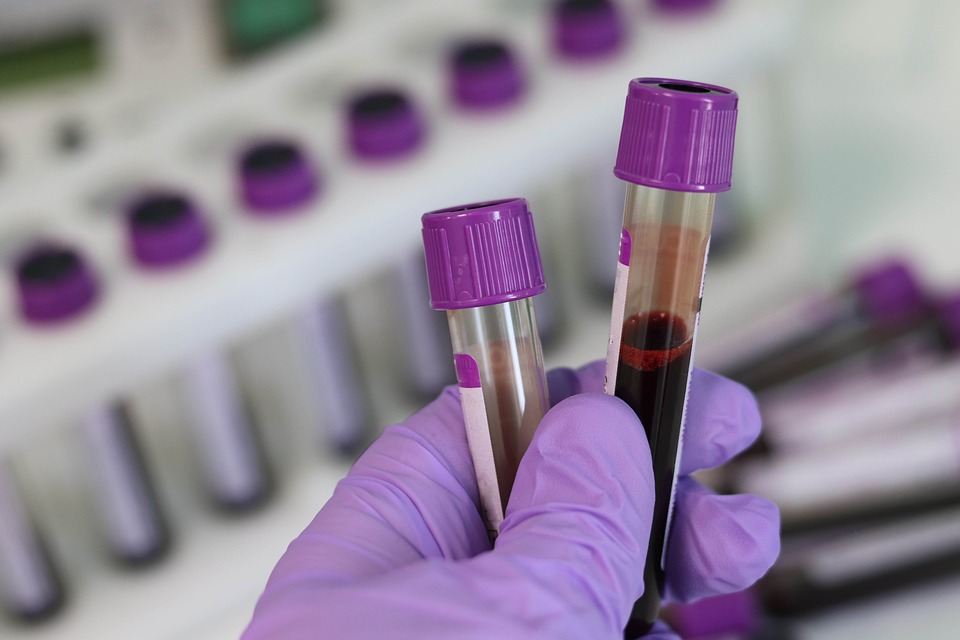
Pictured: The infected blood scandal saw over 4,000 patients affected.
Of that group of over 4,500, around 1,200 were infected with HIV, of which around just one in five are still alive.
Although he declined to provide numbers of those affected “to ensure that no patient identifiable information is disclosed”, the Health Minister confirmed in writing that, as Jersey “mirrored” the UK’s haemophilia treatment procedures, some islanders had been given infected blood.
“Hepatitis C virus remained undiscovered and therefore no diagnostic test had been developed to identify Hepatitis C infection in otherwise healthy blood donors until 1991/1992. Roll-out of routine Hepatitis C testing for Jersey blood donors occurred a few months ahead of roll-out in the UK,” he explained.
The Minister added that there were some difficulties for those affected in gaining compensation.
Pictured: Deputy Richard Renouf, Health Minister.
“The manufacturer of Haemophilia treatment materials used in Jersey was primarily the UK National Blood Transfusion Service (NBTS) and its associated manufacturing arm called BioProducts Laboratory (BPL). Both NBTS and BPL were covered by Crown Immunity until 31st March 1991, meaning that these organisations were protected from legal proceedings.
“Obstacles to Haemophilia patients securing redress in the past included difficulty in establishing which batch of Haemophilia treatment was responsible for infection, out of hundreds or thousands of batches used to treat an individual over 20-plus years, plus the issue that the primary sources of infected material used by both UK and Jersey patients held Crown Immunity at the relevant time.”
Some patients infected with Hepatitis C were given “one-off or recurring payments” via a scheme set up in 2004 known as the Skipton Fund.
Deputy Renouf said that there was no centrally recorded number of how many Jersey patients had accessed this fund, but that some had been assisted in their claims by local consultant medical staff.
The UK Infected Blood Inquiry is currently considering whether that compensation is appropriate or sufficient – findings which Deputy Renouf said would be given “careful consideration” in Jersey.
The Minister also provided reassurance that action had been taken since the blood contamination scandal first came to light, including better preventative measures, gene therapy for haemophilia patients, introducing the Hepatitis B vaccination and the use of antiviral clearance therapy.
Comments
Comments on this story express the views of the commentator only, not Bailiwick Publishing. We are unable to guarantee the accuracy of any of those comments.