

A group of 10 “high-utilisation patients” are currently costing Jersey's Health Department up to £4.2million every year, as a result of being passed “pillar to post” around the system.
The revelation came from the Group Managing Director of Health, Rob Sainsbury, who said that he was looking to reduce these costs by developing a better patient experience as part of the new 'Jersey Care Model'.
His comments were made during a Scrutiny hearing with the Health and Social Security Panel - chaired by Deputy Mary Le Hegarat - which is currently reviewing the model proposed by the government to lighten the hospital's load by improving prevention and making local healthcare more community-based.

Pictured: Rob Sainsbury, Group Managing Director for the Department of Health and Community.
While being quizzed about the “big priorities” of the new model, Mr Sainsbury said the goal was to improve patient experience and coordination between services to avoid spiralling costs.
He said a number of high-risk patients, who access health services frequently, are being passed “pillar to post” around the health and care system, which is pushing up the Health Department's spend.
“They are going between social care, between different physical specialties, between mental health and primary care and not having continuity,” he told the Panel.
“They’re having multiple assessments, multiple opinions and they are not having good case management coordination and their outcome is often left to institutional focused care either secondary care, the hospital, or within the care home environment.”

Pictured: Caroline Landon, Director General for Health and Community Services.
In addition, he said that the “top 10 high utilisation patients” are using up resources worth up to £4.2million, as they are “going around and around and around”, having as many as 20 assessments done before ending up in long-term care.
Mr Sainsbury said the poor connectivity between physical and mental health services is also costing the department money and that it needs to target the “high intensity, high cost, poor outcome patient group”.
Caroline Landon, the Director General for Health and Community Services, said the current system is so “complex and muddled” that the Health Department does not have a “clear line of sight to all our patients”.
“What we need to get to it’s that position of wrapping around all our patients wherever they are and working collaboratively with all the providers whereas at the moment we are all working in a bit of a melée,” she added.

Pictured: The Jersey Care Model aims to preserve the hospital for those who absolutely need it.
Mr Sainsbury said one of the targets of the model was to make sure the hospital is preserved “for those patients who absolutely need specialist hospital-focused intervention”, rather than being occupied by “patients who are medically fit and don’t need to be there”.
“For the community part of our sector, we really want that part to pick up and to manage patients to live a more independent life where they don’t have one choice only, which is predominantly to go into long-term institutional care,” he added. “We want them to have more community care in their own usual place of residence.”
He said the government will not be asking volunteers to provide services and organise care, but rather invest in community services and commission “voluntary providers with paid services” in a similar way to Community Trusts in the UK.
Mr Sainsbury said the Health Department wants to preserve “vulnerable specialities” in the hospital and even introduce more – such as cancer care – so that islanders don’t have to leave the island to be cared for.
“Our model really is about right place, right environment at the right time for the person,” he said.
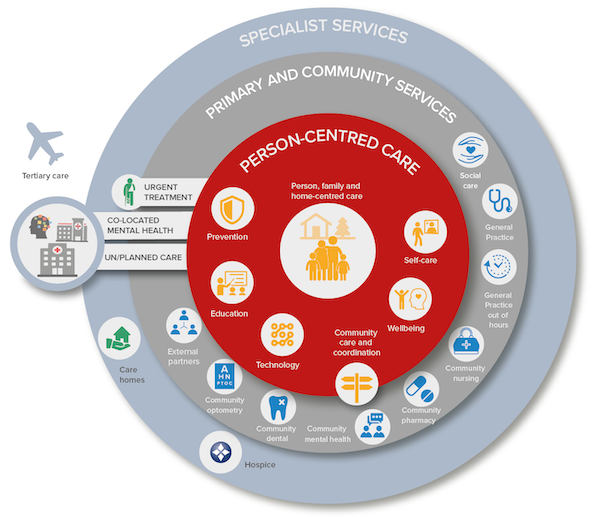
Pictured: The new care model proposed by the Government.
It is hoped that changing the delivery of services at the hospital will help release money to deliver care in the community. However, the Health Minister, Deputy Richard Renouf could not confirm how much money would be saved or exactly how, explaining that health planners would do so in a report to be released in late March.
“To me it is obvious that there will be costs that can come out of the hospital,” he said. “If we are delivering services differently and the hospital is not bringing people in that don’t really need to be in that setting then, they are costs saving there.”
Mr Sainsbury said that investing at the lower level and coordinating the care better would lead to better financial outcomes.
“At the moment we are going from zero to 100 very, very quickly and we’re effectively going from an informal or formal care network that fails and there is nothing that can stop it from catapulting towards a very expensive type of care, either a hospital or a care home or a very expensive package of care,” he explained.
“At the moment, most of our resources - we see it in mental health - is set up at the point of crisis, at the point of dealing with crisis rather than trying to stop the crisis from happening.
“We really hope the Jersey Care Model will say if you invest in this part of the pathway you will reap significant benefit in avoiding that really highly costly part at the end."
Comments
Comments on this story express the views of the commentator only, not Bailiwick Publishing. We are unable to guarantee the accuracy of any of those comments.