


Health says that an increase in reporting of ‘safety events’ over the past two years demonstrates an improved safety culture because staff “feel able to be open and transparent” when they occur.
A patient ‘safety event’ is defined as any "unexpected or untoward event that has a short- or long-term detrimental effect on any person".
Health and Community Services’ recently published inaugural ‘Quality Account’ report for 2022 reveals that there were 4,542 safety events last year – up from 4,057 in 2021.
The vast majority of reported events resulted in no harm or a low level of harm to patients or staff.
643 events were accidents that ‘may or did result’ in personal injury, and of those 487 were slips, trips or falls. Most of these – 71% – resulted in no harm, and 27% in low harm.

Pictured: Slips, trips or falls were common safety events.
Last year, there were also 486 pressure ulcers reported. Health says that reducing that number is a high priority in 2023.
32 ‘serious incidents’ were reported in 2022, including two ‘never events’, which are incidences “that are preventable where guidance or safety recommendations that provide strong systemic protective barriers are available at a national level and have been implemented by healthcare providers”.
Both related to ‘wrong site surgery’.
In its first Quality Account, Health says it is committed to learn from serious incidents.
The report states: “HCS promotes a strong safety culture that ensures learning occurs from safety events to support the delivery of high-quality care.
“When things go wrong, it is vital events are recorded to ensure learning can take place. By learning, we mean people working out what has gone wrong and why it has gone wrong, so that effective and sustainable actions are then taken locally to reduce the risk of similar events occurring again."
It adds: “Serious Incidents in health and social care are rare, but it is acknowledged that systems and processes have weaknesses and human error can occur.
“It is essential that as an organisation we can recognise harm and the potential for harm and undertake swift, thoughtful and practical actions in response ensuring there are opportunities for learning and improvement, ultimately reducing the risk of recurrence.”

Pictured: In its first Quality Account, Health says it is committed to learn from serious incidents.
Health’s Quality Account is intended to “inform the public of the quality of the services we provide”.
The report adds: “This account demonstrates our commitment to provide islanders with the best quality healthcare services. It also encourages transparency about our service quality and helps us to develop ways to continually improve.
Introducing the report, former Chief Officer Caroline Landon, who left Health at the end of March, said: “2022 was a year in which we tackled waiting lists and were subject to close scrutiny about our culture.
“We have a significant engagement workstream underway to address some of the cultural issues and this is progressing well.
“We have also made great inroads into better capturing data through our patient tracking list (waiting list).
“We ensured dental care for children was a key focus, partnering with private local dentists to address waiting lists and reassure parents.
“We have continued with our screening programmes and have re-opened the rehabilitation unit at our Overdale location.
“We now have access to a new Neonatal Unit as part of our ongoing maternity refurbishment. We have delivered our winter plan and participated in the Island-wide response to major incidents.”

Pictured: The former Chief Officer, Caroline Landon, left Health at the end of March.
She added: “The pandemic presented us with operational challenges, but the ambition of our highly skilled, kind and expert workforce which makes up HCS remains consistent; to ensure that our services are there for Islanders of all ages, providing care in the right place, at the right time, to all who need it.
“We know islanders need services which work for them and fit in with their lives.
“We will continue to focus on integrated care services and build on work already delivered in this area. We want islanders to be able to access the service they need when they need it.”
As it is the first Quality Report, there are no full-year statistics to measure against. Also, Health stress that direct comparisons with the NHS are not always possible.
The report establishes ‘Quality Improvement Priorities’ for this year, as well as highlight successes and examples of good practice within HCS.
When it comes to Patient Safety targets, some are ‘zero incidence’ so, for instance, there were 45 incidences of category 3 or 4 pressure ulcers (on a six-category scale) with a target of none, so that particular issue is firmly ‘red’ in Health’s RAG traffic-light system of prioritisation.
Health says that reducing the number of pressure ulcer incidences is a key priority for 2023.
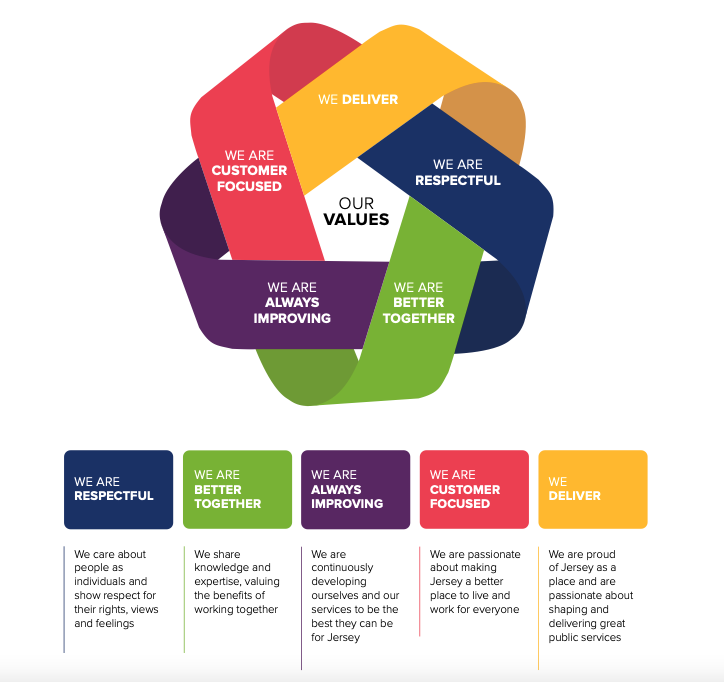
Pictured: HCS's core values, which are listed in its first Quality Report.
Other ‘Red’ lights include preventing and controlling bacterial infection in the Hospital. Again, the official ‘acceptable’ target is zero but, for instance, there were 11 cases of Clostridium Difficile and five cases of e-coli in 2022.
Health says that the expectation that a target of zero for all conditions is “not realistic and under review”. It says it will be looking at trends and “aiming for a year-on-year reduction in numbers until they plateau at an acceptable rate”.
When it comes to ‘Patient Experience’, and specifically waiting lists, 44.83% of patients were waiting more than 90 days for their first outpatient appointment in 2022, slightly better than the baseline of 46.4%.
Health wants that figure to be less than 25%, noting that waiting times were severely impacted by the Covid pandemic.
There is also a Red light in the RAG rating when it comes to patients with learning disabilities, specifically the percentage who have had a physical health check in the last year.
The average over 2022 was 56%. The benchmark in the NHS, released in December, is that 80% of patients should have had health checks, so HCS has some work to do.
Health says that the Quality Account should “assure patients, members of the public and stakeholders that, as a healthcare organisation, we are scrutinising the services we provide, particularly focusing on those areas that require the most attention”.
Comments
Comments on this story express the views of the commentator only, not Bailiwick Publishing. We are unable to guarantee the accuracy of any of those comments.