


It was recently suggested that Jersey's Health Department would be declared bankrupt if it was a UK council – so, after years of overspending, what is being done to get finances back on track?
From boosting productivity to finding ways to generate more income, Express took an in-depth look at the £35m challenge ahead...
The Health Department (HCS) has had long-standing issues with overspending. The Treasury has injected it with cash several times, including £2.7 million reserve funding to tackle waiting lists alone, part of £5 million promised in the 2023-26 Government Plan.
They were “read the Riot Act” by Treasury Minister Ian Gorst in September, with threats that they might not receive the funding they are counting on, should they not save as much as they are promising.
More recently, Andy Jehan resigned from his post as Assistant Chief Minister, citing "serious concerns" about the amount of money spent on the new board recruited to oversee the service.
A document presented to senior leaders in HCS stresses it is “essential” for the department to save the money, or they risk their funding for next year.
In a large service like HCS, employing around 4,000 people, doing this will be a huge challenge – and bed-blocking, waiting lists, and having to use expensive private facilities for people moving out of the Hospital are just some examples of inefficiencies with a very high cost.
“Key clinical services” like Medicine, Surgery, Women and Children, and placements and packages in Mental Health and Social Care are all areas struggling with overspending.
In its current precarious position, the department has given itself until the end of 2025 to stabilise its finances. They certainly have their work cut out for them...
Work on putting together a Financial Recovery Plan started in the spring of this year and HCS finally entered the 'Delivery' phase of the plan in October.
Its first goal is to save £3 million by the end of the year, followed by £12 million in 2024 and £10 million in 2025.
This initial £3 million saving is essential – with Treasury Minister Ian Gorst saying in September that he need the department to bring their spending down and adding: “If I'm absolutely honest, I will only have the certainty that they are getting it under control, if they deliver the £3m saving that they've said they will by the end of this year.
“So, they're still going to be overspent massively in 2023, by around £25m. I've given them lots of money this year, including an extra £5m [to get waiting lists down]. Only this month, they told me, they would make a saving of £3m this year. And until I see that saving, I won’t have the confidence that islanders would expect of me.”
Taking a front-seat role in the plan is Obi Hasan, a member of the 'Change Team' parachuted in to help transform the struggling service. He is the team's financial lead, and has been working full-time since April.
“We went through a period of understanding the problem, connecting and speaking to a lot of people,” he told Express.
“In particular, the clinicians. Of course the exec team, but a lot of the clinicians and operational staff, frontline people, to understand the real issues.
"Walking the floor too, Chris [Bown, interim chief officer of HCS] did that a lot. I've done that and all the Change Team have done that… And that gave us a sense of where things needed to improve, where things were going wrong, what needed to improve.”
The result of their research was deciding to bring on KPMG to put together the recovery plan.
“It’s a plan that describes, over a very deliberate three-year period, how to keep quality of services as well as the money at the same time, working with each other to turn around what has become a large deficit in the health system,” Mr Hasan explained.
“What are the choices we have to make in the short term to do so? And how do we optimise the money that we have available, which has increased, to stabilise the services that are looking very fragile at the moment?”
According to the Financial Recovery Plan – or the 'FRP', as Health officials are calling it – the department has a £35 million underlying overspend.
Of this sum, it is £25 million they plan to cut down on: £3 million by the end of 2023, £12 million in 2024 and £10 million in 2025.
Had they continued as before, the department was on track to overspend by £29 million in 2023. There is also an additional £6 million of funding that they won’t get again next year – leaving the department with a £35 million problem to solve.
Should they reach their £3 million savings goal – and Mr Hasan said he is “cautiously optimistic” – they will have brought that deficit down to £26 million by the end of 2023.
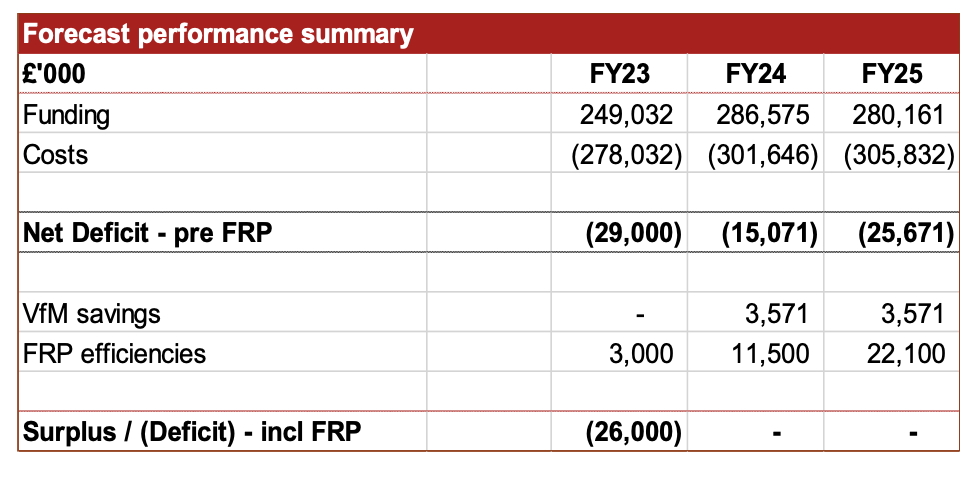
Pictured: The FRP calculates that efficiencies will save the department £3 million by the end of the year
Mr Hasan accepted that the level of savings required was extremely high.
He went on to say: “This is not cuts to services. This is cutting up wastage to use the money better to deliver the services that we've got.”
He said that certain "core values" underpinned the plan – primarily, that quality of care and the department's financial situation should improve in tandem.
This might sound contradictory – and Mr Hasan acknowledges that NHS boards in the UK have made drastic cuts, with quality of care going downhill, but he noted: “There is an intelligent way of doing it, and that’s the way to do it.
"What we're doing is removing waste to use the money better to serve the public.”
The FRP is made up of seven different 'workstreams'.
Some look to the future – digital health, for example, means replacing trips to the UK with remote consultation, or letting patients go home earlier while being able to monitor them.
“It’s not one we’re going to get to quickly,” Mr Hasan said.
Work has started on some of the bigger tasks, contributing, hopefully, to the £3 million goal.
Mr Hasan describes this as “what islanders know as ‘people are stuck in hospitals with nowhere to go’” – with 21 extra beds currently open because everywhere else is full.
Making up one of the largest chunks of the savings, the department needs to get a grip on “inefficient processes” that have been identified.
“It’s patients coming through the hospital being treated efficiently without delays, or with minimal delays, and then going out appropriately to a better setting.
“Hopefully do it at home or into domiciliary care, or into secondary or community care. And doing that efficiently, removing delays.”
This section of the plan will save the department between £1 million and £3 million over the three years.
This year, Mr Hasan said, the spend on locum agencies is going to be around £25 million – paying for 190 agency staff in total.
Slow hiring processes and difficulty finding staff led the department to use agencies, though the cost is high. Of the £25 million spent on locums, around half goes to the agency.
“If I hire them permanently, I’d end spending £13 million – for the same service.”
The service delivered by locums is not as good as hiring permanent staff, Mr Hasan explained.
“If you have your own staff employed, who work day in, day out, they're committed to the island, they're not contractors, they’re committed to the island and live here, they’re working in the same team, they know the team, they cover for each other, they build relationships. You’re going to get a better quality of service, that's just called teamwork. You don't get that with temporary staff.”
Not all of the department’s hiring processes are in HCS’s control, he added.
Making it attractive for people to come to the island and hiring quickly – these are areas where shared services, like government HR, need to help, Mr Hasan said.
Theatre efficiency is about bringing down waiting lists for surgeries, Mr Hasan explained.
“Within the theatre time we are using, we are losing a lot of time as well.”
It’s not just the surgeries themselves that get delayed: assessments and surgery preparation all see delays. The “Golden Patient” process, Mr Hasan said, would put the patient first and make sure the whole procedure goes smoothly.
Checking in on the patient – and reminding them to show up on the day – is expected to help with waiting lists, as is having a streamlined process the day of the operation.
“So if you want to start your theatre at 08:30 in the morning, you've got to make sure you've done the consent by 7.30, 8 o'clock you're ready to roll, by 08:30, you’re there, knife to skin.
“That takes organisation and time. Somebody needs to be on point managing that all the time, making sure this is happening, everything's lined up whilst that patient is being anaesthetised.
“As the procedure goes into recovery, somebody needs to make sure the next patient is ready and the same thing has happened.
“They're organised, they're there. And the list is organised fully. And it's running to time and schedule.”
Operating theatres tend to run two three-hour sessions every day – and Jersey is no exception.
Improving processes would mean, according to Mr Hasan, that instead of fitting two or three patients into each session, they might be able to do four or even five.
Buying drugs, prostheses, equipment, continence products and more represents £80 million pounds for Jersey’s health system.
“All these things have a lot of money attached to them,” Mr Hasan explained.
Having identified the top 20 contracts (including “some very large ones” and with more to look at in future years), he said: “We’re going through methodically, looking what value for money we’re getting.”
They will need to be renegotiated and new suppliers found where necessary. Generic drugs that are just as efficient as the branded version can be up to 10 times cheaper, Mr Hasan explained, and that is work that Jersey hasn’t done in recent years.
Jersey benefits from a partnership with the NHS’s supply chain, he added, which it can tap into to benefit from the prices the NHS has secured.
“These are kind of things that we haven't done and we’ve found these opportunities to do a lot more a lot faster… we're working really close to the pharmacy and our chief pharmacists, who need resourcing.
“We're supporting the remote resources to deliver that as well.
“All the savings pay for themselves many times over.”
Mr Hasan sees income generation as “a big opportunity” in Jersey, where the public purse would benefit from more income from private patients who have the money to spend on health insurance but go to the UK or elsewhere for treatment.
When Mr Hasan asked staff in the radiography department to find ways to bring down the 53-week waiting list for MRI scans, clinicians suggested using the second scanner – which was a back-up should the first machine fail – full-time.
This needs investment, bringing in staff who could man the second machine, but the investment would pay for itself, staff said.
“We trusted them, we invested the money, we allowed them to have a second scanner and invested in hiring more staff to do it,” Mr Hasan said.
The idea was for the private patients using the scanner to pay for the extra staff.
Eight weeks later, the waiting list had been reduced to 11 weeks. The waiting list for private patients then reduced from six weeks to two weeks.
“Before Christmas, our commitment is to bring it down to six weeks for the public. And by choice, on demand, for private. Hopefully we're on target to achieve that.”
But Mr Hasan promised that trying to generate more income can’t mean prioritising richer patients, stressing that waiting lists have gone down for both groups.
“The leadership that we have in place now, we're absolutely committed to the public benefit, because it's a public service.
“All patients are patients. Whether you’re public or private is irrelevant as far as we're concerned… we treat by clinical urgency.
“We must do both public and private, but we can never do one at the expense of the other. And that works both ways.”
He invited anyone who knows of private patients being prioritised unfairly to raise their concerns at the HCS Advisory Board, saying those would be followed up.
He added: “The financial recovery program is one part of a change program. And culture is another part of it. But they're inextricably linked.”
Mr Hasan admitted the digital health workstream is one for future years.
“It’s not one we’re going to get to quickly,” he said, adding that a programme has been identified that would allow people to have consultations digitally instead of flying to the UK, delivering some advisory services remotely, or even remotely monitoring patients who will then be able to go home earlier.
“Those are all possibilities, but we’ll come to that in year two,” he said.
First, the department needs to meet its '£3 million in three months' challenge. The success of this initiative will have an important bearing on future funding, and, importantly, morale in the department.
Mr Hasan added: “How we exit this year into next year, that's really important, because that will set the tone and the direction or what what is to come. It's a psychological barrier for us to hit.
“We are cautiously optimistic that we will be able to deliver the £3 million this year.”
A recent Government blog quotes a Radiology Clinician as saying: “…such that the atmosphere in the department has been transformed, from one of doom and gloom, to a ‘can do, will and must do’ one. Everyone is now extremely positive and walking round with a spring in their step and for that we are all truly, truly grateful. That’s what we in the Radiology department want to do. The best for our patients and colleagues and this is empowering us to do so.”
Then, the bigger challenge will be to meet targets for the next two years.
Mr Hasan continued: “Whether it becomes a trend that we can maintain next year remains to be seen. That's the challenge, my challenge and the challenge for this organisation that we maintain.”
He reiterated the £3 million, £12 million and £10 million goals, adding that the last £10 million are for areas that were never properly funded and will continue to receive government cash.
“So that would solve our 35-million-pound problem.”
Health leaders “read the Riot Act” over budget overspends
Too many managers in Health? No, says report...by Health
Bill for "constipated" Health management rises to £10m
ANALYSIS: As the next budget looms... What should we expect?
FOCUS: £234m for a project yet to lay a foundation stone...and may take 12 more years?
Comments
Comments on this story express the views of the commentator only, not Bailiwick Publishing. We are unable to guarantee the accuracy of any of those comments.