


GPs have torn into the Government over its "somewhat fatalistic" pandemic handling, accusing it of adopting mask use too slowly, creating a £14m Nightingale Wing that couldn’t be properly staffed, and endangering the lives of care home residents.
In an extraordinary letter sent to a panel of politicians reviewing the island’s covid response, the Primary Care Body said the Government had used terminology that "downplayed the seriousness of covid" and “mirrored many of the mistakes in the British Isles.”
Among those “mistakes”, they argued, was a failure to protect the island’s “most vulnerable patients” – including some who “were initially sent back to residential/nursing homes without having been tested for the virus.”
This, they claimed, led to the “rapid spread within institutional care and a consequent high proportion of deaths of patients being cared for”.

Pictured: GPs said that the lack of testing of vulnerable patients had led to “rapid spread" within care homes "and a consequent high proportion of deaths".
“The situation was compounded by the lack of PPE, which was denied by the Government, and extended to carers working in patients’ homes,” the GPs added.
“Given recent changes in advice, the PPE recommendations provided to health care workers in the community were, in retrospect, insufficient in many scenarios.”
According to Government figures, there have been 29 covid-related deaths in care homes, three in St. Saviour’s Hospital and three in domestic properties since the beginning of the pandemic.
The group also noted how the implementation of physical distancing and mandatory mask wearing had been slower in the island, and suggested “further exploration” around the timing of lockdowns, which they argue could have differed from “the pattern in the British Isles” to what they described as “considerable advantage”.
“Jersey could also have introduced border controls at an earlier point and maintained them for a longer period emulating many other jurisdictions,” they argued.
“Jersey lifted the lockdown at the beginning of summer 2020 for largely economic reasons.
"It would be important to ascertain if the perceived benefits outweighed the fact that there were further deaths, particularly following emergence of the Delta variant, and islanders spent Christmas in relative isolation whilst our sister island enjoyed near normality.”
The GPs also called for a review into the building of the Nightingale wing, which cost more than £11m to put up and was never used.
"The number of those infected never approached a point where it would have been feasible to use it and the ability to ever staff it appropriately must be questioned," they said.

Pictured: The Nightingale wing was demolished this summer.
According to the group, a more “cost-effective option” would have been to create ‘virtual hospitals’ where patients would be given pulse oximeters and other means of self-monitoring - but this was never seriously explored.
The Primary Care Body was also critical of the way the Urgent Treatment Centre, which opened in April 2020 and closed in July 2020, was operated.
The Panel described it as “an excellent temporary addition to the initial fight against covid” and praised the work of the general practitioners who “proved themselves to be an invaluable part of health service provision."
However, they said there had been “little support” from the Emergency Department, even when it was “quiet”, and doctors were seconded to the UTC despite nearly all hospital services being suspended.

Pictured: The Urgent Treatment Centre, which opened in April 2020.
“Some patients attending the UTC would clearly have been more appropriately triaged to the ED, e.g. road traffic accidents and stroke patients,” the GPs said.
“There was an expectation of patients being managed within the UTC when it was not necessarily the most appropriate place for them to be cared for. The UTC was not adequately resourced when GP numbers were reduced despite patient safety concerns being raised.”
The panel also noted how the GPs' “commendable work” had been recognised by islanders but had not received any “official acknowledgement” from Government, with a number of awards having been given “almost exclusively to HCS employees."
They added that concerns over the financial stability of practices as they returned to ‘business as usual’ as well as over the affordability of healthcare for patients had been dismissed, whilst contract issues had been difficult to resolve and led to delays in payments.

Pictured: The GPs said they were “surprised” to have been denied the opportunity to be part of the covid vaccination programme.
They also said they had been “surprised” to having been denied the opportunity to be part of the covid vaccination programme, despite general practices and community pharmacies having administered 30,000 influenza vaccines within five weeks.
Praise was, however, reserved for Deputy Medical Officer of Health, Dr Ivan Muscat.
Having been “thrust to the fore as an expert in infectious disease", he was lauded for having continued to provide "cogent advice throughout the most difficult of times."
While noting its development was slower than on the mainland, the Primary Care Body said Jersey's equivalent of the NHS Track and Trace App "eventually proved useful and effective."
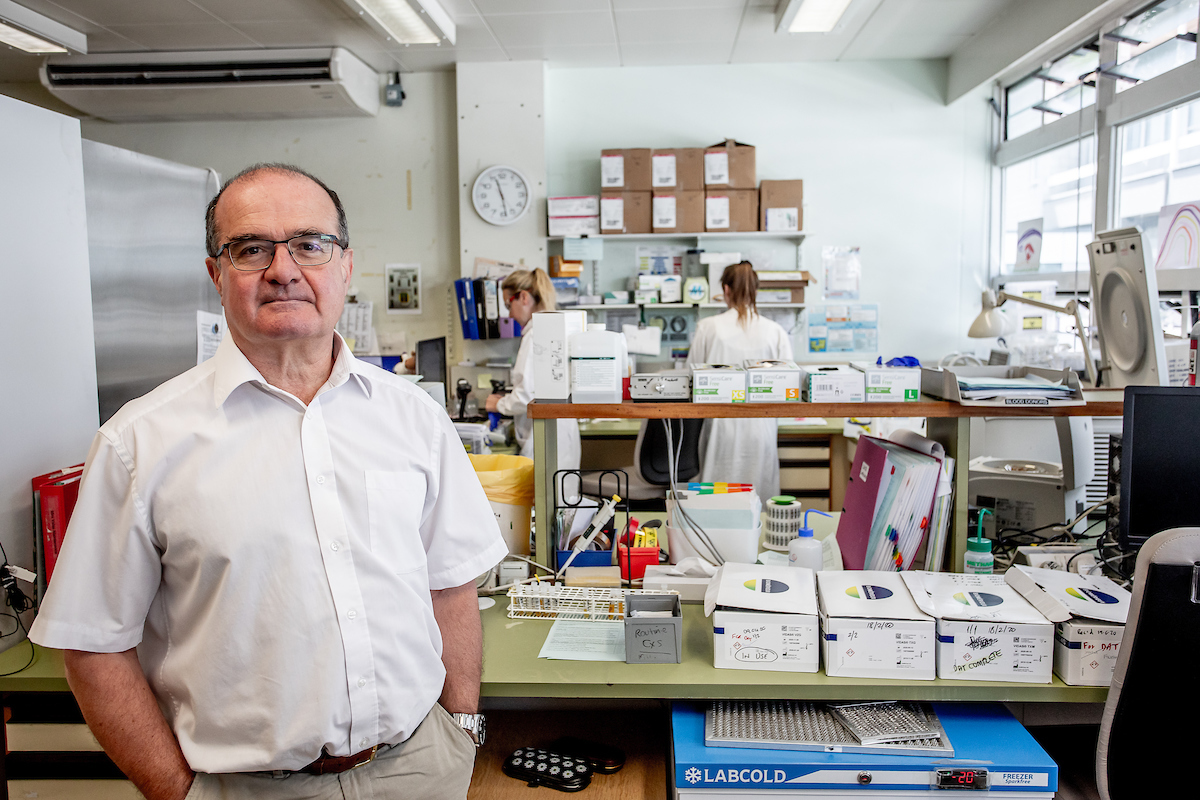
Pictured: Dr Ivan Muscat was praised by the Primary Care Body.
As well as the healthcare response, politicians leading a review into the Government's handling of covid - the Public Accounts Committee - are also investigating Ministers' and officials' decision-making, management of public finances, support to businesses, and procurement and supply chain management.
They continuing to accept evidence from individuals and groups, and any submissions can be sent via its online form, or by emailing scrutiny@gov.je.
Comments
Comments on this story express the views of the commentator only, not Bailiwick Publishing. We are unable to guarantee the accuracy of any of those comments.