


Official guidance has been drawn up to help medical professionals make the "incredibly difficult decision" which covid-19 patients should get critical care if the health service is overwhelmed as case numbers peak.
The ‘Ethical Framework’ – as the guidance is known - was shared by the government yesterday afternoon.
In some countries crippled by covid-19, doctors in stretched hospitals have reported how life-or-death decisions have had to be made based on age or other crude measures.
To avoid this, Jersey’s most senior clinicians have developed a set of guidelines to help them with “prioritising patients for care and rationing scarce resources”, should it become impossible to help everyone with covid-19 in need.
Video: The Chief Minister, Health Minister and Medical Director introduced the new framework at a press conference yesterday.
There is no cure for the illness – only time, and, in some extreme cases, the provision of additional oxygen via a ventilator of which there are currently fewer than 30 on the island.
The “guiding principle” of the framework, which has full political backing, is that patients with “higher clinical likelihood of benefit” will be given precedence over those less likely to make a full recovery or enjoy a longer life expectancy.
This means that, in a worst case scenario, patients deemed to have a lower chance of survival could have a ventilator withdrawn from them or be moved from the ICU in favour of someone else.
Decisions will be made by a ‘triage committee’, rather than doctors or nurses on the frontline, in order to “buffer” them from the potential “debilitating distress” arising from such decisions.
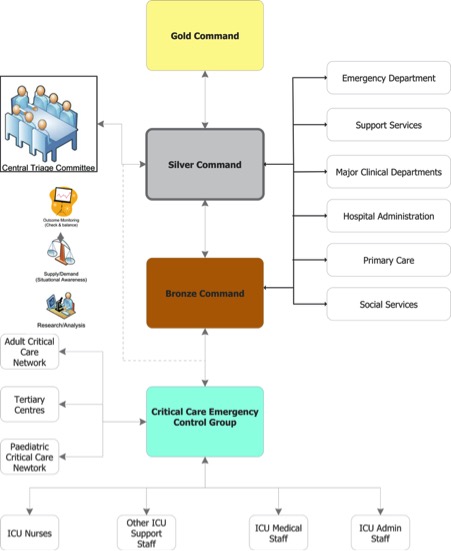
Pictured: The Health Department's structures for managing the triage process.
The system, which also aims to spread the burden among numerous people rather than single individuals, also allows for doctors and nurses to become ‘advocates’ for patients and, where necessary, appeal certain decisions.
Although there should be no discrimination on the basis of age alone, the document explains that a “fair innings” approach would be “justifiable” in the case of a choice between “a 12-year-old and a 64-year-old both with similar disease severity and pre-existing conditions”.
Admitting the process is "very controversial", Medical Director Patrick Armstrong explained that the clinicians behind the strategy were keen to ensure the document had the full support of Ministers "so my critical care colleagues taking those decisions are not left living those decisions".
Asked by Express how far lifestyle factors - such as smoking or weight - will play a part in life-or-death decisions, Mr Armstrong replied: "My critical care colleagues will assess every patient on their own merits and they will work out as best that they can – it’s not an exact science – how likely that individual is going to benefit.
"Yes, lifestyle choices may have led to a point where health is such that they’re less likely to benefit, but someone would not be turned down on the basis that they smoke. It will be on how likely they are to recover given any intervention that is provided."

Pictured: Mr Armstrong explained that lifestyle factors may play a part in decision-making.
He added: "I would rather sadly also make the point that when people get to the point of requiring critical care intervention, particularly ventilation, the evidence that we’re seeing from other countries is that your survival rate is about 50% once you get to that point, so you are already very critically ill at that point."
According to the document, global evidence suggests that of patients infected with covid-19, around 15% have a severe illness, and 5% a critical one.
Although there is no official treatment for the illness, Mr Armstrong assured that staff at the hospital - which will be backed by an additional 180 beds based at the Millbrook ‘Nightingale’ facility as the crisis reaches its peak in May – will work hard to reduce numbers of islanders in need of emergency care.
“While we have no treatment for the actual virus, we can support patients during the course of the illness by providing oxygen therapy, intravenous fluids, nutritional support, other vital organ support – for example, for the heart and the kidneys – as well as antibiotics in the event that secondary pneumonia is developed.
“By supporting people in this way, we can reduce the need for critical care.”

Pictured: The 'Nightingale' facility currently under construction at Millbrook. (Gary Grimshaw)
Such traumatic decision-making has led to a spike in cases of mental health problems, such as PTSD, and even suicides among doctors, nurses and other health workers globally.
To reduce any resulting emotional harm, all those involved in the process locally will be able to access "bespoke psychological support" and "spiritual support" in the form of chaplaincy services should they need it.
CLICK BELOW to read the document in full...
Comments
Comments on this story express the views of the commentator only, not Bailiwick Publishing. We are unable to guarantee the accuracy of any of those comments.