


It’s time for an "open debate" about whether Jersey should have its own National Heath Service, Jersey's senior intensive care doctor has told Express in a candid interview touching on life, death and how his perspective on medicine has been changed by the pandemic.
Today marks 365 days since the first case of covid-19 was officially recorded in Jersey.
In a series of interviews this week, Express has spoken to islanders about how the virus crisis has changed their outlook.
First, we speak to Intensive Care medic, Anaesthetist, Deputy Medical Director and Vaccine Prioritisation Panel Chair, Dr Paul Hughes…
The hospital wasn’t seized by a fit of sudden panic when covid reached Jersey, but rather there was an undercurrent of fear that swept through the staff community, underscoring their daily duties as they ‘kept calm and carried on’.
“Everyone was fearful. We haven’t really had a pandemic in anyone’s lifetime, so everything was unknown,” Dr Hughes recalled.
“People were fearful and people were concerned, and there was a conflict there between their duties as people working in health to protecting themselves and their families. People were having showers before they went home because they were scared of bringing stuff home… In my area, in intensive care, we all thought we might die, we literally thought we might die.”

Pictured: Staff in the hospital were "fearful", Dr Hughes recalled.
But Dr Hughes - a Royal Air Force Medical Officer for 16 years, leaving as a Wing Commander - was steeled somewhat by his military background: “I was prepared to get shot, so I was prepared to catch the virus.”
He continued: “I deployed to Kosovo – the Kosovan War – I worked in a field hospital in the Kosovan war, deployed to the second Gulf War and worked in a field hospital in Southern Iraq. I also spent my Air Force career mainly bringing patients back from Afghanistan and various war zones.
“I had to use the same skills as you would do, briefing a team and going into an uncertain environment and the leadership element was really important – everyone supporting each other and talking about certain things, starting to express anxieties.”
But, despite having “seen a lot of stuff”, including being “shot at while picking up people in a helicopter”, the consultant of 20 years still describes dealing with covid as one of the most “challenging” and “surreal” experiences of his life.
The fortitude instilled by his military background was unable to reduce the pain involved in telling covid patients they’d have to be put to sleep and ventilated or informing islanders that their loved ones had passed away.
“We form relationships with the patients we’ve lost on ITU. The patients are fearful, because they know that they’re on ITU and they know that this is really serious. The nature of the illness is that they’re not delirious so they’re actually fully aware of what’s going on and to have a conversation with someone saying, ‘I’m going to have to put you off to sleep and put a tube in’, the patient knows there’s a good chance they’re going to die.”

Pictured: Despite his military background, Dr Hughes said he still found many moments on the ITU difficult to deal with.
He added: “When people are really really ill on critical care, we normally have the family around them at the bedside, and as we’re doing things, we’re talking to the family. That’s been missing. That’s really hard in that you’re almost the nurse and medical staff having to be completely the patient’s advocate and some of the phone calls I’ve had to make where people have died and I’ve had to tell the ones on the phone that’s happened, I’ve never had do to before.”
Those feelings were supplemented by a sense of frustration that there was no specific treatment to offer.
“30% of patients who come to Critical Care die on average. So it’s not that we’re not used to patients dying on Critical Care, but it’s normally that that happens after a long period of many interventions of different things, and we haven’t got a big suite of interventions to help people when they get really really sick with coronavirus.”
Above all, Dr Hughes says he was blindsided by the “injustice” of the virus.
“It’s almost like survivor guilt. I’ve treated almost every sick coronavirus patient on the island and I’ve also been carrying on giving anaesthetics, and I haven’t caught it and now I’ve been vaccinated so I’m not going to get it… It’s really confusing, how can I not have caught it? The injustice of it… There were people who were shielding and they got it. It’s a cruel, cruel illness.”
Despite this, Dr Hughes says that his memories of the past year are filled with happier moments of laughter, togetherness and achievement.
Throughout, he was not only buoyed by thank you cards from the families of patients he had helped, but the “remarkable things” completed in a short space of time like expanding the ITU capacity “four to five times”, and the solidarity, fortitude and cooperation shown by hospital staff - ranging from doctors and nurses to the cleaners to the porters.
Pictured: Dr Hughes says it's the people that make the hospital, not the building.
“Porters taking patients up and down the hospital – they were scared. I was alright in ITU because I had all the [PPE] on, but the porters just had a mask and a pin… but they did it, and they were still as cheeky,” he smiled.
“Everybody pulled together and it really emphasised the fact that the hospital is actually a community. It’s really interesting in the context of conversations around the big, shiny new hospital on the hill – it doesn’t matter about the building. I’ve annoyed people by saying that. If I wanted a hospital, I could ask someone at military college to put a 400-bed hospital on People’s Park in two days’ time. It’s not about the hospital, it’s about the people and the caring.”
It was a feeling many in the wider island community appeared to share. But that swell of appreciation for health staff’s hard work throughout the pandemic - reflected in rainbows, fundraising, food and gift donations, and a regular ‘clap for carers’ - gave Dr Hughes pause for thought.
Those thoughts crystallised as he drove to work during lockdown - “the roads were clear, it took five minutes to get there” - and would spot an NHS flag flying on Victoria Avenue.
“With the NHS flags, on Jersey, we don’t have a National Health Service. What that said to me is that people like the philosophy of a National Health Service, and that’s something we really need to start an open debate about on the island."

Pictured: Dr Hughes thinks it's time for a debate about whether there should be a 'national health service' in Jersey.
He added: “If people want to talk about a ‘National Health Service’, well, a national health service for Jersey means everybody has equal access to healthcare, free at the point of access.
“I’m a Welshman, that’s what Nye Bevan said, and I’m a Socialist, so I firmly believe that equity of access to healthcare is really, really important. It’s a fundamental, social construct that I think really matches with the concept of Jersey and the parishes, and the community as an island.
“There’s lots of debate on the new hospital, but that’s just a building. If we really want a national health service then we need to have conversations about paying for GPs. I’m not supposed to get overtly political as a doctor, but equity of access to healthcare – and we’ve seen it with coronavirus, not so much here – but in the UK it’s clear that those who live in disadvantaged communities, non-professionals, have had a much worse outcome. And they’re the ones who are going to be made unemployed. They’re the ones who are going to really struggle. The children within those families are going to really struggle for the rest of their lives.”
As he set about the grim task of writing the ‘Ethical Care Framework’ - which laid out how medical professionals should make the “incredibly difficult decision” which patients should get critical care if the health service became overwhelmed - Dr Hughes says several questions surged into his mind.

Pictured: A statue of Nye Bevan in Cardiff.
“When I was doing that, I started to think, this is inconceivable. How can we, as a civilised society ever be faced with a situation where I’m going to have to turn down healthcare for someone?”
Such questions echoed themes explored in Chapter 5 of Nye Bevan’s 1948 work, ‘In Place of Fear’, in which he lays out a vision for a National Health Service.
“He talks about it being a fundamental part of society, and how can a decent society not accept that everyone should have access to health? It’s not a commodity.
“If you can’t do it on such a wealthy island like Jersey with really great facilities, there’s something wrong with the way the conversation is happening in public. I think sometimes we’re getting a bit distracted with the 'hospital on the hill’ and all the noise around it, but actually there’s a real opportunity to get this social conversation going.”
Dr Hughes later added: “There’s [a suggestion] on the island that this hospital depends on private income for it to run – I’m not sure that’s right. I’ve got nothing against private practice. That’s alright, so long as we ensure that an elderly lady living on her own in a dilapidated cottage in St. Ouen has equal access to healthcare as someone who lives in a 27-bed mansion in St. Martin.”
In this instance, everyone investing in making healthcare free at the point of access would mean equal protection for the minority of islanders with little means. It might sound a ‘radical’ concept to some, but covid community spirit, Dr Hughes says, has already proven that the majority is capable of acting in the interests of the few.

Pictured: The island community has already demonstrated it can act in the interests of a smaller group by taking actions during the pandemic to protect the elderly and vulnerable.
“Everything everyone’s done in terms of isolation and lockdown has been to protect the elderly. So you as a young person has gone through that to protect the elderly. So, as an island, yes, we are prepared to think about the wider community in terms of our actions.
“From an economic and political point of view, we should continue that debate. Who on the island do we need to protect?”
He added: “We’ve come together as a community to fight this thing, and I think it would be a shame if when it all disappears in June – let’s hope it does – we don’t continue this social conversation… We need to draw upon the experience of covid and talk about the social importance of caring for each other.”
As Chair of a panel in charge of considering islanders’ applications to ‘jump the queue’ in the vaccination process, Dr Hughes does, however, have a concern that this community spirit may have started receding.
“You see the cracks appearing with people saying, ‘I’m really important, I need the vaccine.’ I understand that, I’m not being critical, but it’s shifting back from, ‘We’re all in this together’ to, ‘I’m more important than you.’
“It would be a shame to go back to people behaving as individuals rather than people feeling part of something bigger.”
To try and move the conversation forward in terms of what quality healthcare for the benefit of all islanders could look like in future, Dr Hughes has penned a ‘Quality Strategy’, which is currently sitting with the Health Minister for consideration.
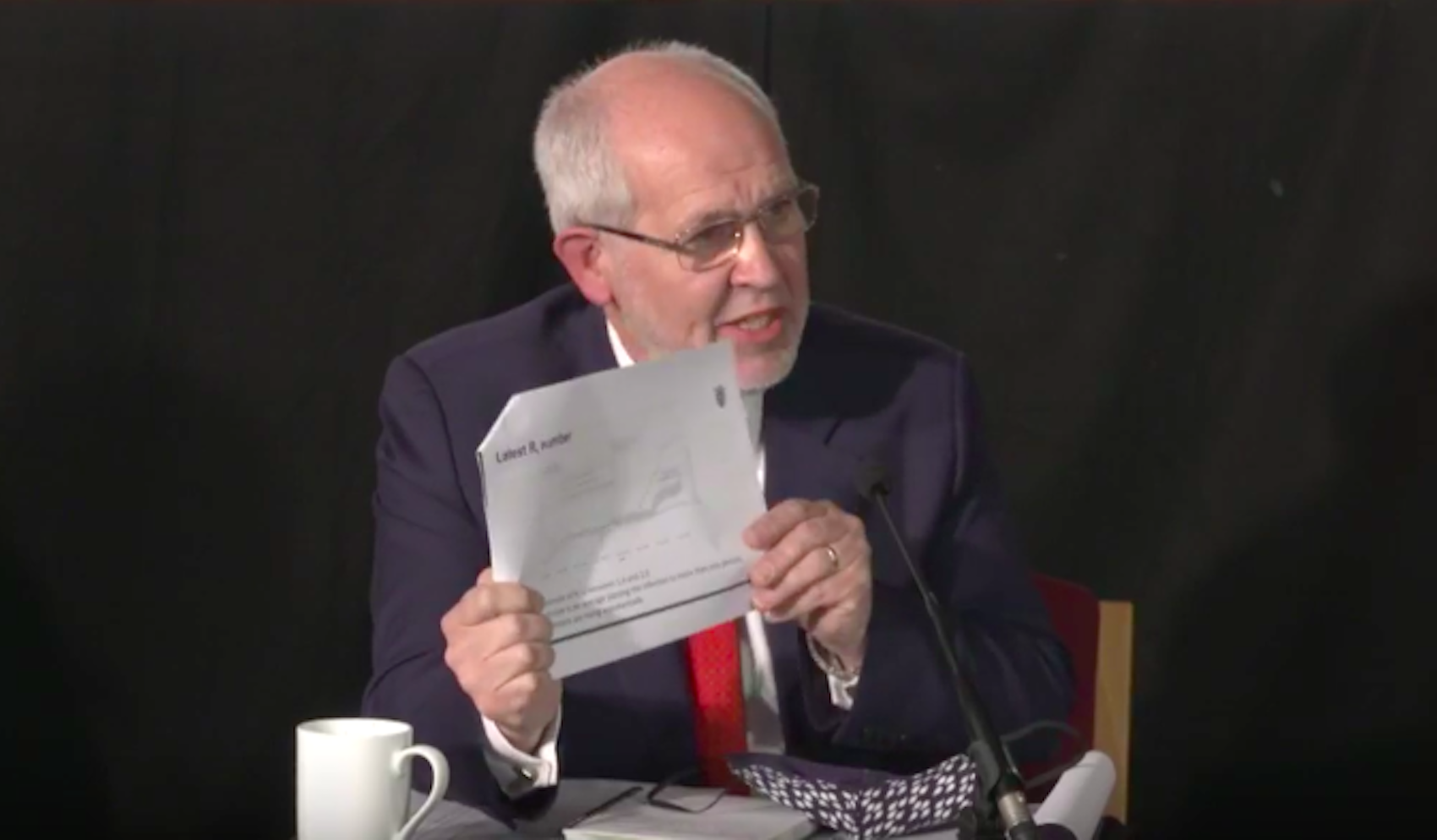
Pictured: Dr Hughes has written up a Quality Strategy which is before the Health Minister, Deputy Richard Renouf, for consideration.
"I’ve been Medical Director in other places. Because a lot of hospitals in the UK are inspected, they’re inspected using criteria using the elements of ‘quality'.
“‘Quality’ is defined as ‘safe’; ‘effective’, that means it’s evidence-based, you’re doing the right thing; ‘efficient’ means you’re doing it and not wasting money; ‘equitable' means that everybody’s got equal access to that resource; and 'patient-centred'.
“It’s not about someone like me thinking, 'I’ve got this clever drug I’m going to give you', it’s about what does the patient need? They’re worldwide definitions of what quality is, and it’s never been properly described in that way here in terms of the Government papers.
“There have been improvement plans and strategies, but they’ve never turned round and said, actually, this is what we’re going to deliver. It’s making these definitions clear.
“The next step is getting the Health Minister and the political debate around committing to that, which is what everybody else has done.”
In ensuring Jersey can reach all of these standards, the new Jersey Care Model, which aims to ensure that more services are available in the community, is a good place to start, Dr Hughes says.
“[Covid] changed how I feel about medicine… The inability to treat this disease I think is important both in my personal feeling and a bigger conversation about what medicine does in society… To a certain extent, medicine has made these people who have died – the ‘at risk’ population – we’ve created that, we’ve made them vulnerable.”
According to Dr Hughes, that’s because society’s understanding of health has become overly hospital-centric: “We wait until someone is irretrievable, and then we try and help. It’s better creating the environment where we don’t need help in the first place.”
“What is healthcare? Healthcare isn’t all the flashy stuff I do, with my machines and gadgets and drugs – health is something different to that. Health is meeting people’s needs.”
He later adds: “…People like me and hospital doctors think the hospital is 'where it’s at', and more and more money is being spent on that – and things that actually make a long-term difference, like education and housing, have been neglected.”

Pictured: Ensuring islanders have access to good quality housing and education should be considered as components of healthcare, according to the medic.
According to Dr Hughes, contrary to what some may believe, it may be the “social worker or foster parent that contributes greater to public health” than any doctor.
A natural consequence of the global tendency to work on getting better at treating illness rather than focusing efforts on community prevention is that costs will continue going up - something every jurisdiction, ranging from the UK with its NHS to the US and its private model, is battling against.
“Our population is ageing... the amount of chronic disease in the community is going up – how do we make ends meet? Healthcare costs will increase and sooner or later we’ll run out of money. It will suck all the money out of schools, Social Security – and it’s not just us, it’s everywhere. The answer is a community-based healthcare system.”
He is clear, however, that the Jersey Care Model is not about cost-cutting: “What it absolutely isn’t is cutting costs and taking things that we have in the hospital now and plonking them in a parish hall.”
The benefits of such a model come into focus when considering the challenges of Jersey’s ageing population.
“Once an elderly patient comes into hospital, it’s really difficult to get them out,” he reflects. “Actually, if you spent time and money with occupational therapists and social workers and dealing with the housing issues for an elderly patient and providing Meals on Wheels and companions, so they’re not lonely, it’s better than eventually letting them deteriorate so that they eventually if they have to come into hospital, they’ve reached the point where it’s difficult.”
Dr Hughes adds: “Medicine isn’t all about technology or doing more, it’s about talking to patients, meeting their needs, rather than convincing them to have what I can provide, which is a very interesting distinction.”
Society - including doctors - may have to go through a process of psychological realignment if such an “ambitious” shift is to work, though - something that Dr Hughes acknowledges.
“With General Practice, there’s a real opportunity there. If people can get over the hurdle that they’re private companies, they have got a real opportunity to actually lead this.”
The other way to open minds to new ways of doing healthcare is to look at setting up something similar to the ‘Bevan Commission’, where experts hold public discussions - “not a debate, it’s not asking you to reach any conclusions” - about “the issues that are really difficult”.
Building on achievements to be "really proud" of, like the "bold step" of keeping schools open for children's mental health and its "state-of-the art and probably best-in-the-world" vaccine programme, leading the way with a community-focused healthcare model could give the island an opportunity to establish itself on the global stage, Dr Hughes says.
It could also help Jersey in establishing links with other jurisdictions to ensure islanders have access to top quality services offered elsewhere - something the pandemic led Dr Hughes to reflect on.

Pictured: Jersey should work on linking up with other jurisdictions.
“One of the lessons that we had was when we were thinking about being overwhelmed was that we were on our own. And if we were overwhelmed, who is going to help us?
"Actually, that shouldn’t be true. The reality is that medicine – some of the complicated medicine, which is different to the caring medicine – there’s no way we can do that. So we should have partners in the UK.
“One of the lessons we need to learn is we can’t be self-sufficient in terms of healthcare – given the choice of having something here or going to an expert centre, most people would go to an expert centre. We need to build links with other places in terms of sharing expertise and with that comes research.”
At the beginning of the pandemic, Jersey offered to take part in two covid treatment trials: one involving drugs and another relating to oxygen flow devices.
In the end, the former was “too complex to get through the ethical processes”, while, fortunately and unfortunately, there was only one patient eligible for the latter.
Nonetheless, “it’s gone noted in the UK that we were trying to contribute.”
Perhaps, in time, the island could even consider its own Medical School. It has already started training mental health nurses, and some doctors too.
The future may be paved with “wicked” problems, Dr Hughes concludes, but it is also extremely “exciting”.
“We’ve got real opportunities to do fantastic things. Focusing on care, focusing on looking after each other is the start. And we’re heading in the right direction.”
Comments
Comments on this story express the views of the commentator only, not Bailiwick Publishing. We are unable to guarantee the accuracy of any of those comments.